NEMT Cost of Care Study: How Does Transportation Impact Healthcare Spending?
Research has shown that nearly four million Americans miss or delay medical care every year because they lack reliable transportation. While non-emergency medical transportation (NEMT) services typically account for less than 1% of total healthcare spending, consistent access to healthcare vastly enhances member health outcomes and leads to dramatic cost savings for health plans.
Transportation is inexpensive compared to the high and rapidly growing cost of healthcare. NEMT services funded by Medicaid and Medicare ensure members who do not have a reliable personal means of transportation are able to access their medical appointments. By providing cost-effective NEMT services, health plans decrease the impact of chronic disease, reduce the cost of inpatient medical treatment, prevent missed appointments, and remove barriers to care.
But one question we often hear from our NEMT clients is “how does transportation impact healthcare spending?” To reach a conclusion, MTM Health conducted a NEMT cost of care study using data made available by our client partners.
NEMT Cost of Care: The Data
During our study, MTM Health reviewed more than 43,000 member records to determine if the ongoing cost of care was impacted by the regular use of Medicaid-funded NEMT. Specifically, we studied high-risk diabetic populations over the age of 12 who utilize NEMT to access their healthcare appointments in five states: Florida, Iowa, Maryland, Texas, and the District of Columbia.
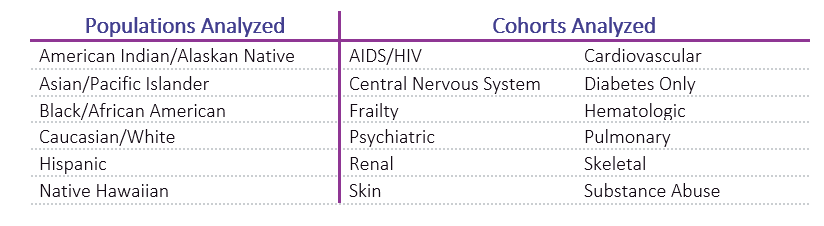
We looked at the data set in three ways: first, we analyzed the population as a whole, then we analyzed specifically the Caucasian population, and then we analyzed minority populations as a group. The table below details the specifics of the populations analyzed.
During analysis, we reviewed the average cost of care and average medical claim billed units per member over a period of 12 months. We specifically compared high-risk diabetic members who utilize Medicaid-funded NEMT services versus members who do not utilize NEMT services. To complete the analysis, secondary cohorts were isolated and analyzed, along with Type 1 and Type 2 diabetic members.
NEMT Cost of Care: What We Found
Our study shows that among the populations we analyzed, when the Medicaid-funded NEMT benefit is utilized as a regular part of a member’s care management strategy, their average cost of care for identified cohorts is significantly lower. Demonstrated across all populations and cohorts was a reduction in the average cost of care and/or reduction in billed units.
Interestingly, we found that while 57.7% of NEMT-eligible members studied came from minority populations, only 37.6% of actual NEMT utilizers were minorities. In comparison, 42.3% of NEMT-eligible members studied were Caucasian, while 62.4% of actual NEMT utilizers were Caucasian. Our data and findings conclude that while fewer minority members utilize their NEMT benefit to get to medical care, NEMT-utilizing minority members have a lower average cost per care than NEMT-utilizing Caucasian members.
Our NEMT cost of care findings firmly support the continued use of NEMT services, as it is more cost-effective to transport a member to preventative care rather than waiting for a serious health condition to arise. By offering the NEMT benefit to transportation disadvantaged populations, health plans can effectively:
- Remove transportation barriers
- Prevent missed medical appointments
- Decrease the impact of chronic disease
- Reduce the costs of inpatient medical treatment
- Save substantial healthcare funding
Categories
- Alaina Macia (39)
- Employee Wellness (19)
- ETO Newsletter (64)
- Events (70)
- MTM Health eNewsletter (83)
- News & Events (710)
- Technology (2)
- Tradeshows (57)
- Uncategorized (17)
- Webinars (15)